Menopause and Joint Pain: Causes, Relief, and Management
Nov 18, 2024
Menopause is a natural biological process that marks the end of a woman's reproductive years, typically occurring in their late 40s to early 50s. While it brings about various physiological changes, one of the less discussed yet significant issues is the connection between menopause and joint pain. Many women report experiencing joint discomfort during this transition, which can be attributed to hormonal fluctuations, lifestyle changes, and other factors. Understanding this connection is crucial for managing symptoms effectively and maintaining a healthy, active lifestyle.
Understanding Menopause and Its Impact on Joints
What Happens During Menopause?
Menopause is defined as the time when a woman has not had a menstrual period for 12 consecutive months. This transition is marked by a decrease in the production of hormones such as estrogen and progesterone. These hormonal changes can lead to various symptoms, including hot flashes, mood swings, sleep disturbances, and joint pain.
The Role of Estrogen in Joint Health
Estrogen plays a vital role in maintaining joint health. It helps to regulate inflammation and supports the production of collagen, which is essential for joint integrity. When estrogen levels drop during menopause, women may experience increased inflammation and a reduction in collagen production, leading to joint pain and stiffness. Studies have shown that women undergoing menopause are more likely to report joint pain, particularly in the knees, hands, and hips.

Common Types of Joint Pain During Menopause
Women may experience various types of joint pain during menopause, including:
Osteoarthritis: This degenerative joint disease is characterized by the breakdown of cartilage, leading to pain and stiffness. It is more prevalent in postmenopausal women due to hormonal changes and aging.
Rheumatoid Arthritis: An autoimmune condition that can be exacerbated by hormonal fluctuations, leading to increased joint pain and inflammation.
Tendonitis: Inflammation of the tendons can occur, causing pain around the joints, particularly in the shoulders, elbows, and knees.
Bursitis: Inflammation of the fluid-filled sacs (bursae) that cushion the joints, leading to pain and swelling.
Risk Factors for Joint Pain During Menopause
Several factors can increase the risk of joint pain during menopause:
Age: The risk of developing joint issues increases with age, as the body's natural repair mechanisms slow down.
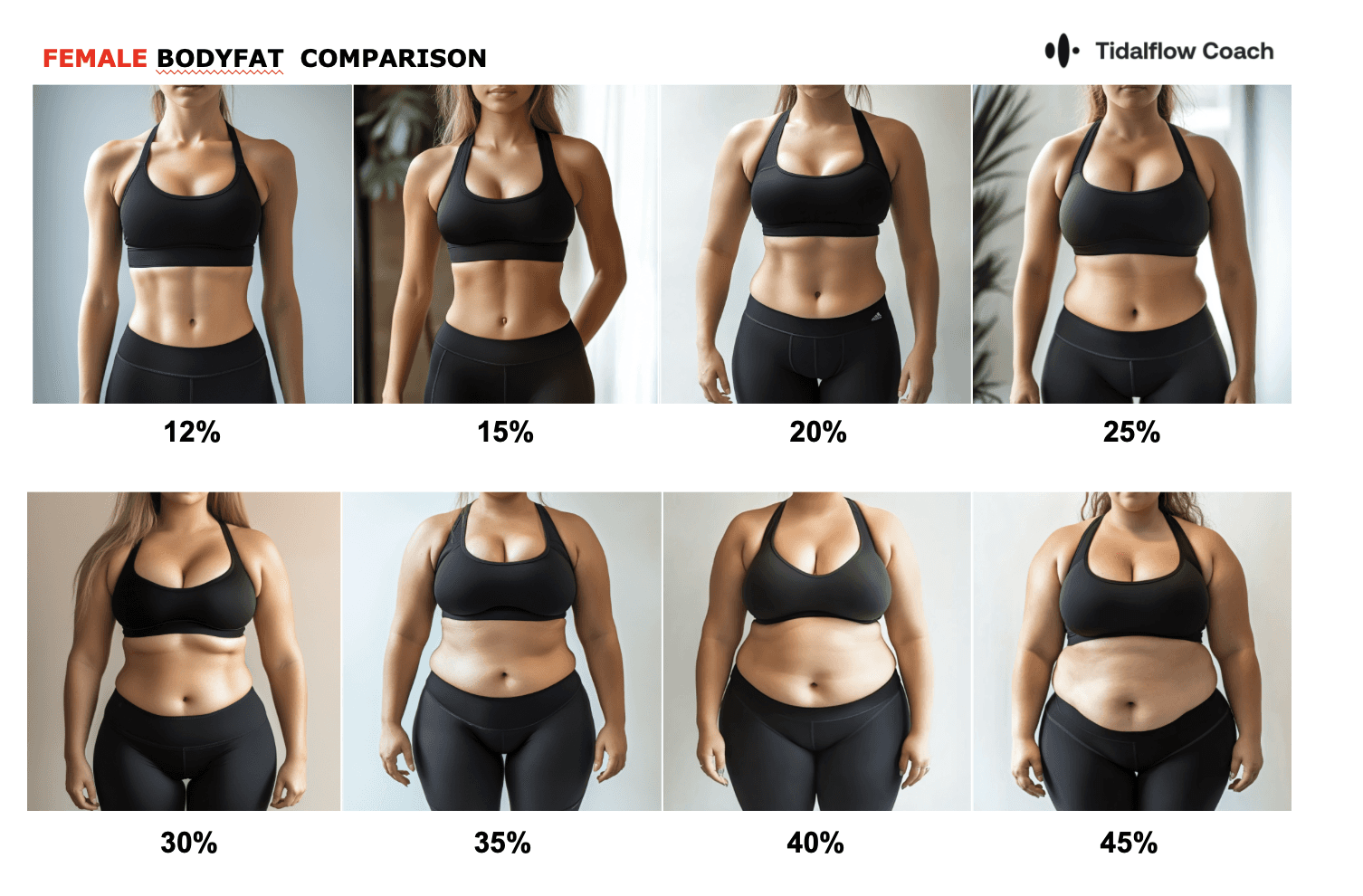
Weight: Excess weight can put additional stress on the joints, particularly the knees, hips, and ankles.
Genetics: A family history of joint issues or certain genetic factors can predispose women to similar problems.
Physical Activity: A sedentary lifestyle can weaken muscles and joints, increasing the risk of pain and injury.
Hormonal Imbalances: Fluctuations in hormone levels, particularly estrogen, can contribute to joint pain and inflammation.
Effective Relief Strategies for Joint Pain During Menopause
Lifestyle Changes
Making certain lifestyle changes can significantly alleviate joint pain during menopause:
Regular Exercise: Engaging in low-impact exercises such as walking, swimming, cycling, or yoga can help maintain joint flexibility and strength. For more targeted strength training, check out our article on top lower body pull exercises for maximum strength and power.
Weight Management: Maintaining a healthy weight can reduce stress on the joints. Consider tracking your progress with our water creatine intake calculator to optimize your hydration and performance.
Balanced Diet: Incorporating anti-inflammatory foods such as fatty fish, nuts, leafy greens, and berries can help reduce inflammation. Additionally, ensure adequate calcium and vitamin D intake for bone health.
Stress Management: Stress can exacerbate joint pain and inflammation. Practice relaxation techniques like deep breathing, meditation, or yoga to manage stress levels.
Physical Therapy and Complementary Therapies
Working with a physical therapist can provide personalized exercises and treatments to strengthen muscles around the joints, improve flexibility, and reduce pain. They can also guide you in proper body mechanics to prevent further injury. Additionally, complementary therapies such as acupuncture, massage, and chiropractic care may provide relief for some women.

Medication and Supplements
Over-the-counter pain relievers such as NSAIDs (e.g., ibuprofen, naproxen) can help manage pain and inflammation. Additionally, supplements like glucosamine, chondroitin, and omega-3 fatty acids may provide relief for some women. However, it's essential to consult with a healthcare provider before starting any new medication or supplement regimen, as they may interact with other medications or have side effects.
Hormone Replacement Therapy (HRT)
In some cases, hormone replacement therapy (HRT) may be recommended to help alleviate menopausal symptoms, including joint pain. HRT can help restore estrogen levels and reduce inflammation, potentially providing relief for joint discomfort. However, HRT is not suitable for everyone, and it's crucial to discuss the risks and benefits with a healthcare provider.
The Role of AI in Personal Training and Joint Pain Management
As you navigate the challenges of menopause and joint pain, consider leveraging technology to enhance your fitness journey. Getlila's AI personal training solutions can provide customized workout plans that accommodate your specific needs and limitations. Our platform offers personalized coaching that adapts to your progress, ensuring you stay on track without exacerbating joint pain. Learn more about how AI personal trainers can transform your workout routine.
Additionally, Getlila's AI-powered app can help you track your symptoms, monitor your progress, and provide personalized recommendations for managing joint pain during menopause. By leveraging the power of artificial intelligence, you can receive tailored guidance and support throughout your journey.
Frequently Asked Questions
What helps joint pain during menopause?
Several strategies can help alleviate joint pain during menopause, including regular low-impact exercise, weight management, an anti-inflammatory diet, stress management techniques, physical therapy, and medications or supplements as recommended by a healthcare provider. Hormone replacement therapy may also be an option for some women.
How long does menopausal joint pain last?
The duration of joint pain during menopause can vary from woman to woman. For some, the joint pain may be temporary and subside once hormone levels stabilize after menopause. However, for others, joint pain may persist or worsen over time, especially if underlying conditions like osteoarthritis are present.
What causes joint pain in a 50-year-old woman?
Joint pain in a 50-year-old woman can be caused by various factors, including menopause-related hormonal changes, osteoarthritis, rheumatoid arthritis, tendonitis, bursitis, or other underlying conditions. It's essential to consult with a healthcare provider to determine the specific cause and receive appropriate treatment.
Does lack of estrogen cause joint pain?
Yes, a lack of estrogen can contribute to joint pain. Estrogen plays a crucial role in regulating inflammation and supporting collagen production, which is essential for joint health. When estrogen levels drop during menopause, it can lead to increased inflammation and joint discomfort.
Conclusion
Menopause can be a challenging time for many women, especially when it comes to managing joint pain. By understanding the connection between menopause and joint pain, and implementing effective strategies to manage symptoms, women can maintain an active and fulfilling lifestyle. Getlila is here to support you on this journey with our AI-powered personal training solutions, designed to help you achieve your fitness goals while addressing the unique challenges of menopause. Start your journey towards a healthier, pain-free life today with Getlila.
Ready to Simplify Weight Loss?
Download the Lila app or visit getlila.com to start your journey. Experience the power of an AI-driven approach designed to adapt to your changing body and unique needs. Embrace holistic weight loss with Lila—because you deserve to feel strong, confident, and truly yourself again.
Disclaimer: This article is for informational purposes only and does not substitute professional medical advice. Consult a healthcare provider for personalized recommendations.
You should not have to do it all on your own