When Does Menopause Start? A Comprehensive Guide for Women
Nov 25, 2024
When Does Menopause Start? A Comprehensive Guide to Understanding Menopause
Menopause is a natural and inevitable part of aging for women, signifying the end of menstrual cycles and fertility. It is defined as occurring 12 months after a woman's last menstrual period and typically happens between the ages of 45 and 55, with the average age being 51 in the United States ^1^. While menopause is a universal biological process, the experience can vary greatly among women, both in terms of timing and symptoms.
Understanding when menopause starts, the stages involved, and how to manage the associated symptoms is crucial for maintaining quality of life during this transition. In this comprehensive guide, we delve into the various aspects of menopause, supported by reputable sources, to provide you with accurate and up-to-date information.
The Stages of Menopause
Menopause is not a single event but rather a gradual process that occurs in three main stages:
Perimenopause
Menopause
Postmenopause
Perimenopause
Perimenopause, also known as the menopausal transition, marks the period leading up to menopause. This stage can begin as early as the mid-30s but more commonly starts in the 40s. During perimenopause, the ovaries gradually produce less estrogen, leading to hormonal fluctuations that cause changes in menstrual cycle length and frequency.
The duration of perimenopause varies among women; it can last from several months to up to 10 years, with an average of around four years ^2^. Recognizing the signs of perimenopause is essential for women to manage symptoms effectively and prepare for the onset of menopause.
Common signs and symptoms during perimenopause include:
Irregular menstrual cycles (shorter or longer cycles, heavier or lighter bleeding)
Vasomotor symptoms such as hot flashes and night sweats
Sleep disturbances
Mood swings, irritability, or depression
Vaginal dryness and discomfort during intercourse
Decreased fertility
Changes in cholesterol levels, potentially increasing cardiovascular risk
Menopause
Menopause is officially diagnosed when a woman has not had a menstrual period for 12 consecutive months without other obvious causes ^1^. It signifies the end of reproductive capability due to the ovaries ceasing to release eggs and a significant decrease in the production of estrogen and progesterone ^3^. While the average age of natural menopause is 51, it typically occurs between ages 45 and 55.
Symptoms experienced during perimenopause may persist into menopause and sometimes intensify due to the further decline in hormone levels. It's important for women to consult healthcare providers if they experience any bleeding after menopause, as postmenopausal bleeding can be a sign of serious conditions like endometrial hyperplasia or cancer.
Postmenopause
Postmenopause refers to the years following menopause. Once a woman has gone 12 months without a menstrual period, she is considered postmenopausal ^1^. During this stage, the body adjusts to the lower levels of estrogen and progesterone. While some menopausal symptoms may lessen, others can persist for several years or even become chronic.
Women in postmenopause are at increased risk for certain health conditions due to the decrease in estrogen levels, including:
Osteoporosis: Reduced estrogen can lead to decreased bone density, increasing the risk of fractures.
Cardiovascular Disease: Estrogen has a protective effect on the heart, and its decline may increase the risk of heart disease.
Urinary Incontinence: Weakened pelvic muscles can lead to urinary urgency and leakage.
Vaginal Atrophy: Thinning and drying of the vaginal walls can cause discomfort and increase susceptibility to infections.
Regular medical check-ups and adopting a healthy lifestyle are crucial during postmenopause to manage these risks.
Signs and Symptoms of Menopause
While every woman's experience with menopause is unique, there are some common signs and symptoms to be aware of:
Irregular Menstrual Cycles
During perimenopause, hormonal fluctuations can cause changes in menstrual patterns. Women may notice:
Changes in Flow: Periods may become heavier or lighter.
Changes in Cycle Length: Cycles may become shorter (less than 21 days) or longer (more than 35 days).
Missed Periods: Skipping one or more periods is common.
Spotting: Light bleeding or spotting between periods may occur.
It is important to monitor menstrual changes and consult a healthcare provider if bleeding is extremely heavy or accompanied by other concerning symptoms, as these could indicate other health issues ^4^.
Hot Flashes and Night Sweats
Hot flashes are sudden feelings of warmth, often most intense over the face, neck, and chest, and can cause sweating and reddening of the skin. They are among the most common symptoms of menopause, affecting up to 75% of women. Night sweats are hot flashes that occur during sleep, potentially disrupting sleep quality.
The exact cause of hot flashes is not fully understood but is believed to be related to changes in hypothalamic regulation of body temperature due to hormonal fluctuations ^5^.
Mood Changes
Hormonal changes during perimenopause and menopause can impact neurotransmitters in the brain, leading to mood swings, irritability, anxiety, and increased risk of depression. Women with a history of depression or premenstrual syndrome (PMS) may be more susceptible to mood disturbances during menopause.
Sleep Disturbances
Menopause can contribute to sleep problems, including:
Difficulty falling asleep
Frequent awakenings during the night
Early morning awakening
Insomnia
Sleep disturbances may be exacerbated by night sweats, anxiety, and mood changes. Poor sleep quality can impact overall health and exacerbate other menopausal symptoms.

Vaginal Dryness and Discomfort
Reduced estrogen levels can cause thinning, drying, and inflammation of the vaginal walls, a condition known as vaginal atrophy. Symptoms include:
Vaginal dryness
Itching or burning
Discomfort or pain during sexual intercourse (dyspareunia)
Increased susceptibility to urinary tract infections (UTIs)
These changes can significantly impact quality of life and sexual health.
Cognitive Changes
Some women report cognitive difficulties during menopause, such as:
Memory lapses
Difficulty concentrating
"Brain fog"
These changes may be associated with hormonal fluctuations, sleep disturbances, and mood changes. Research suggests that these cognitive symptoms are usually temporary and improve postmenopause.
Managing Menopause Symptoms
While menopause is a natural process, the associated symptoms can significantly impact a woman's quality of life. Fortunately, there are various strategies and treatments available to help manage these symptoms:
Lifestyle Modifications
Adopting healthy lifestyle practices can alleviate menopausal symptoms and improve overall well-being ^6^.
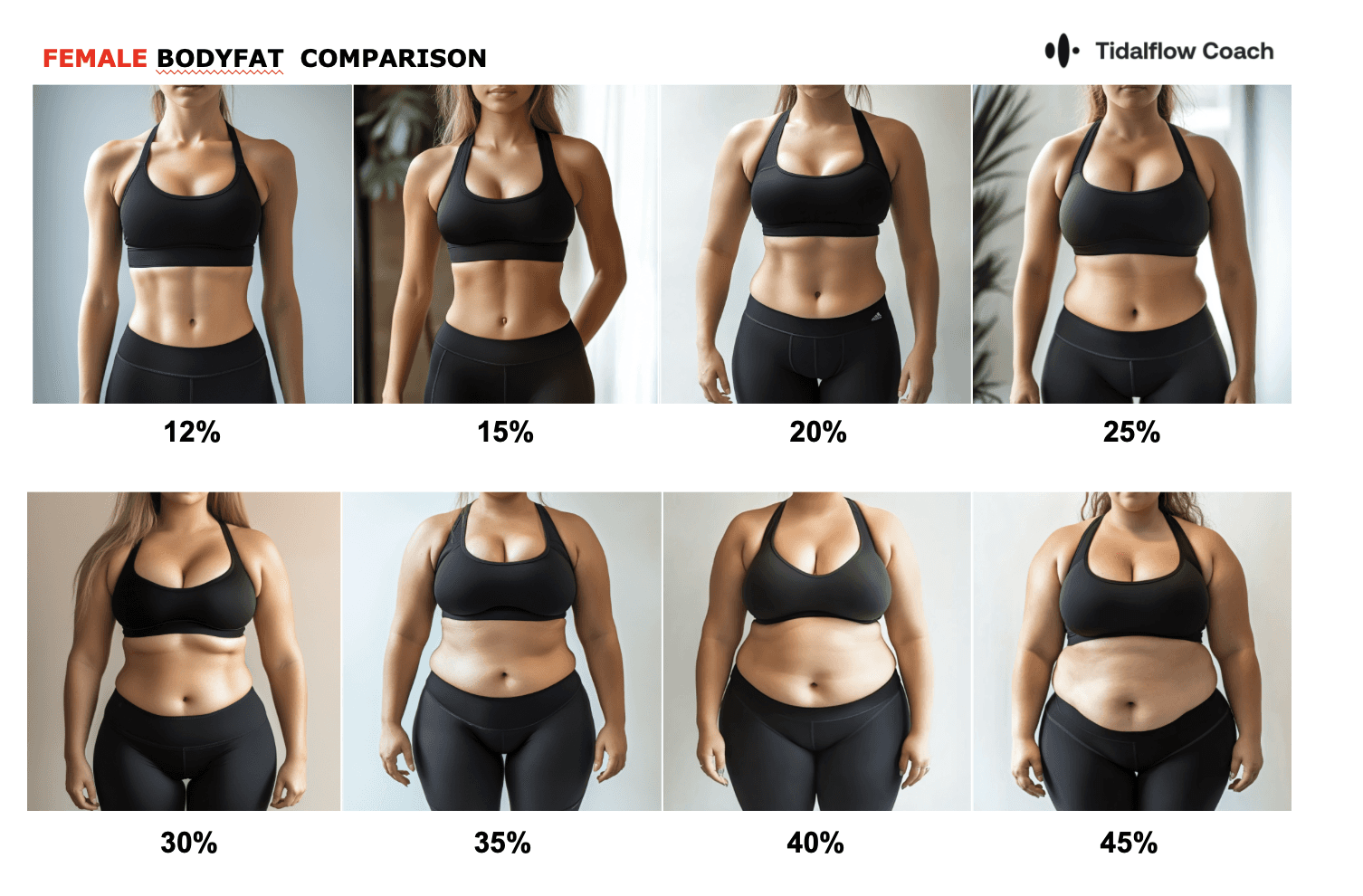
Regular Physical Activity: Exercise can help reduce hot flashes, improve mood, maintain a healthy weight, strengthen bones, and promote better sleep. Aim for at least 150 minutes of moderate aerobic activity or 75 minutes of vigorous activity per week, plus strength training exercises twice a week.
Balanced Diet: Consuming a diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats supports overall health. Including foods high in calcium and vitamin D is important for bone health. Phytoestrogens, found in soy products, flaxseeds, and legumes, may help alleviate hot flashes for some women.
Stay Hydrated: Drinking plenty of water can help reduce bloating and aid in temperature regulation.
Limit Alcohol and Caffeine: Reducing intake of alcohol and caffeine may decrease hot flashes and improve sleep quality.
Quit Smoking: Smoking can exacerbate menopausal symptoms and increase the risk of cardiovascular disease and osteoporosis.
Stress Management: Techniques such as mindfulness, yoga, deep-breathing exercises, and meditation can help manage stress and improve mood.
Hormone Therapy
Hormone therapy (HT) can effectively relieve many menopausal symptoms, particularly hot flashes and vaginal dryness ^7^. HT involves the administration of estrogen alone (for women who have had a hysterectomy) or combined estrogen-progestin therapy (for women with an intact uterus) to prevent endometrial hyperplasia.
Benefits of Hormone Therapy:
Reduction in vasomotor symptoms (hot flashes, night sweats)
Improvement in sleep quality
Prevention of bone loss and reduction in fracture risk
Relief of vaginal symptoms
Risks and Considerations:
Increased risk of blood clots (venous thromboembolism)
Increased risk of stroke and heart disease
Increased risk of breast cancer with long-term use of combined estrogen-progestin therapy ^8^
Possible increased risk of dementia if started after age 65
The decision to use HT should be individualized, considering the severity of symptoms, health history, age, and personal preferences. The lowest effective dose for the shortest duration necessary is generally recommended.
Non-Hormonal Treatments
Several non-hormonal medications can help manage menopausal symptoms, especially for women who cannot take hormones or prefer not to.
Selective Serotonin Reuptake Inhibitors (SSRIs): Low doses of SSRIs such as paroxetine, fluoxetine, and citalopram can reduce the frequency and severity of hot flashes.
Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs): Medications like venlafaxine and desvenlafaxine may also alleviate hot flashes.
Gabapentin: An anticonvulsant medication effective in reducing hot flashes, particularly nighttime symptoms.
Clonidine: A blood pressure medication that can provide relief from hot flashes, though side effects may limit its use.
Vaginal Moisturizers and Lubricants: Over-the-counter products can relieve vaginal dryness and discomfort during intercourse.
Ospemifene: A selective estrogen receptor modulator (SERM) approved for treating dyspareunia due to vaginal atrophy.
Complementary and Alternative Therapies
Alternative approaches may provide symptom relief for some women, though scientific evidence of their effectiveness varies.
Herbal Supplements:
Black Cohosh: May help reduce hot flashes, though studies show mixed results. Long-term safety is not established, and there is a potential risk of liver damage ^9^.
Phytoestrogens: Plant-derived estrogens found in soy and red clover supplements. Evidence is inconsistent regarding their effectiveness in reducing hot flashes ^10^.
Evening Primrose Oil: Traditionally used for menopausal symptoms, but studies have not demonstrated significant benefits.
Acupuncture: Some studies suggest acupuncture may help reduce hot flashes and improve mood and sleep, though more research is needed ^11^.
Mind-Body Practices: Yoga, tai chi, meditation, and deep-breathing exercises can reduce stress and improve overall well-being. They may also alleviate some menopausal symptoms .
Hypnotherapy and Cognitive Behavioral Therapy (CBT): Can be effective in reducing the severity of hot flashes and improving sleep and mood.
It's crucial to consult a healthcare provider before starting any complementary therapies, as some supplements can interact with medications or have side effects.
Maintaining Overall Well-Being During Menopause
Menopause is not just a physical transition but can also impact mental and emotional well-being. Here are some strategies to support your overall health during this time:
Prioritize Self-Care
Self-care is essential during the menopausal transition to maintain mental and emotional health.
Stress Reduction: Chronic stress can exacerbate menopausal symptoms. Techniques such as mindfulness meditation, progressive muscle relaxation, and deep-breathing exercises can help manage stress levels ^12^.
Therapy and Counseling: Speaking with a mental health professional can provide support for mood changes, anxiety, or depression.
Social Support: Maintaining strong social connections with friends, family, or support groups can improve emotional well-being.
Pursue Hobbies and Interests: Engaging in enjoyable activities can enhance mood and provide a sense of fulfillment.
Stay Physically Active
Exercise offers numerous benefits during menopause ^13^:
Aerobic Exercise: Activities like walking, cycling, swimming, or dancing improve cardiovascular health, aid in weight management, and reduce hot flashes.
Strength Training: Lifting weights or using resistance bands helps maintain muscle mass, strengthen bones, and improve metabolism.
Flexibility and Balance Exercises: Yoga, Pilates, or tai chi enhance flexibility, balance, and posture, reducing the risk of falls.
Mental Health Benefits: Regular exercise can alleviate symptoms of depression and anxiety, improve sleep quality, and boost self-esteem.
Consult a healthcare provider before starting a new exercise program, especially if there are underlying health conditions.
Maintain a Balanced Diet
Nutrition plays a key role in managing menopausal symptoms and reducing health risks.
Calcium and Vitamin D: Essential for bone health. Include dairy products, leafy green vegetables, fortified foods, or supplements as recommended.
Protein: Supports muscle mass. Include lean meats, poultry, fish, eggs, legumes, and nuts.
Healthy Fats: Omega-3 fatty acids found in fatty fish, flaxseeds, and walnuts may reduce inflammation and improve heart health.
Fiber: High-fiber foods like whole grains, fruits, and vegetables aid digestion and help control weight.
Limit Added Sugars and Processed Foods: Reducing intake can help manage weight and improve overall health.
Hydration: Adequate water intake is important, especially if experiencing night sweats.
Limit Caffeine and Alcohol: May trigger hot flashes and disrupt sleep.
Seek Support
Building a strong support network can make navigating menopause easier.
Healthcare Providers: Regular consultations can help manage symptoms, monitor health, and provide personalized advice.
Support Groups: Connecting with others experiencing similar challenges can provide emotional support and practical tips.
Educational Resources: Accessing reliable information from reputable organizations can empower women to make informed decisions.
Family and Friends: Open communication about experiences can foster understanding and support.
Embrace the Journey with Personalized Support
Navigating menopause can be more manageable with the right support and resources. Utilizing modern technology, such as AI-powered personal training and wellness applications, can provide personalized guidance tailored to your specific needs.

These platforms can offer:
Customized workout plans that accommodate your fitness level and address menopausal symptoms like weight gain and bone density loss.
Nutritional guidance to ensure a balanced diet that supports hormonal health and overall well-being.
Mindfulness and stress management tools to help cope with mood changes and sleep disturbances.
Progress tracking to monitor improvements and adjust plans accordingly.
By leveraging these tools, you can take an active role in managing your health and embracing this new chapter with confidence and vitality.
Take the first step towards a healthier, more fulfilling life during menopause by exploring personalized wellness solutions that align with your goals.
Frequently Asked Questions
What are the first signs of menopause?
The first signs of menopause often occur during perimenopause and may include:
Irregular Periods: Changes in menstrual cycle length, flow, or frequency.
Hot Flashes and Night Sweats: Sudden feelings of heat, sweating, and flushing.
Sleep Disturbances: Difficulty falling asleep or staying asleep.
Mood Changes: Increased irritability, anxiety, or depression.
Vaginal Dryness: Discomfort or pain during intercourse due to decreased lubrication.
Decreased Fertility: Reduced likelihood of conceiving due to irregular ovulation.
Recognizing these symptoms can help women seek appropriate guidance and support.
What is the average age to start menopause?
The average age for menopause onset is 51 years in the United States, but it can range between 45 and 55 years. The onset of perimenopause, the transition period leading up to menopause, typically begins in a woman's 40s but can start earlier.
Factors influencing the timing of menopause include genetics, smoking status, and certain medical treatments or conditions.
What is the first stage of menopause?
The first stage of menopause is perimenopause, also known as the menopausal transition. During this period, ovarian hormone production becomes erratic, leading to menstrual irregularities and the onset of menopausal symptoms. Perimenopause can last for several years, and it's during this stage that women may begin to experience hot flashes, mood changes, and other symptoms.
Can you get menopause at 35?
While the average age of menopause is 51, some women may experience premature menopause, which occurs before age 40. Menopause at 35 is considered premature and can be due to:
Primary Ovarian Insufficiency (POI): A condition where the ovaries stop functioning normally before age 40.
Medical Treatments: Chemotherapy or radiation therapy for cancer can damage the ovaries.
Surgical Removal of Ovaries: Oophorectomy leads to immediate menopause.
Genetic Factors: Certain chromosomal abnormalities can cause early menopause.
Autoimmune Disorders: Conditions where the immune system attacks ovarian tissue.
Women experiencing menopausal symptoms at a young age should consult a healthcare provider to determine the cause and discuss management options. Early menopause can have significant health implications, including increased risk of osteoporosis and cardiovascular disease.
Conclusion
Menopause is a natural phase of life that marks the end of a woman's reproductive years. Understanding the stages of menopause, recognizing the signs and symptoms, and knowing how to manage them can empower women to navigate this transition with confidence.
By adopting healthy lifestyle practices, exploring treatment options, and seeking support, women can alleviate symptoms and maintain a high quality of life during and after menopause. Remember, each woman's experience is unique, and it's important to work closely with healthcare providers to develop a personalized approach to managing menopause.
Ready to Simplify Weight Loss?
Download the Lila app or visit getlila.com to start your journey. Experience the power of an AI-driven approach designed to adapt to your changing body and unique needs. Embrace holistic weight loss with Lila—because you deserve to feel strong, confident, and truly yourself again.
References
<a id="1">1. </a>Mayo Clinic. (n.d.). Menopause. Retrieved from https://www.mayoclinic.org/diseases-conditions/menopause
<a id="2">3. </a>Office on Women's Health, U.S. Department of Health & Human Services. (n.d.). Menopause. Retrieved from https://www.womenshealth.gov/menopause
<a id="3">4. </a>National Institute on Aging. (n.d.). Menopause. Retrieved from https://www.nia.nih.gov/health/what-menopause
<a id="4">4. </a>American College of Obstetricians and Gynecologists (ACOG). (n.d.). Abnormal Uterine Bleeding. Retrieved from https://www.acog.org/womens-health/faqs/abnormal-uterine-bleeding
<a id="5">5. </a>The North American Menopause Society (NAMS). (n.d.). Hot Flashes. Retrieved from https://www.menopause.org/for-women/sexual-health-menopause-online/causes-of-hot-flashes
<a id="6">6. </a>Harvard Health Publishing. (n.d.). Menopause: Lifestyle Modifications. Retrieved from https://www.health.harvard.edu/womens-health/menopause
<a id="7">7. </a>The North American Menopause Society (NAMS). (n.d.). Hormone Therapy Position Statement. Retrieved from https://www.menopause.org/publications/clinical-practice-materials
<a id="8">8. </a>Women's Health Initiative (WHI). (n.d.). Study Findings. Retrieved from https://www.nhlbi.nih.gov/science/womens-health-initiative-whi
<a id="9">9. </a>National Center for Complementary and Integrative Health (NCCIH). (n.d.). Black Cohosh. Retrieved from https://www.nccih.nih.gov/health/black-cohosh
<a id="10">10. </a>Cochrane Database of Systematic Reviews. (n.d.). Phytoestrogens for Menopausal Symptoms. Retrieved from https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD001395.pub4/full
<a id="11">11. </a>Menopause Journal. (n.d.). Acupuncture for Menopausal Hot Flashes. Retrieved from https://journals.lww.com/menopausejournal/Abstract/2016/04000/Acupuncture_and_moxibustion_for_menopausal_hot.7.aspx
<a id="12">12. </a>American Psychological Association. (n.d.). Stress Management Techniques. Retrieved from https://www.apa.org/topics/stress
<a id="13">13. </a>National Institute on Aging. (n.d.). Exercise and Physical Activity. Retrieved from https://www.nia.nih.gov/health/exercise-physical-activity
Disclaimer: This article is for informational purposes only and does not substitute professional medical advice. Consult a healthcare provider for personalized recommendations.
You should not have to do it all on your own