Genitourinary Syndrome of Menopause: Restoring Well-Being
Nov 20, 2024
Menopause is a natural transition that every woman experiences, marking the end of her reproductive years. While this phase brings about various physical and emotional changes, one condition that often goes unaddressed is genitourinary syndrome of menopause (GSM). This condition, previously known as vulvovaginal atrophy or atrophic vaginitis, affects a significant number of postmenopausal women and can have a profound impact on their overall well-being and quality of life.
Understanding Genitourinary Syndrome of Menopause
What is GSM?
Genitourinary syndrome of menopause is a condition characterized by changes in the vulvovaginal area and lower urinary tract due to the declining levels of estrogen during menopause. As estrogen levels drop, the vaginal tissues become thinner, drier, and less elastic, leading to various symptoms that can significantly affect a woman's physical, emotional, and sexual health.
Symptoms of GSM
The symptoms of genitourinary syndrome of menopause can vary in severity and may include:
Vaginal dryness, irritation, and discomfort
Painful intercourse (dyspareunia)
Recurrent urinary tract infections (UTIs)
Urinary incontinence or urgency
Burning sensation during urination
Vaginal itching or discomfort
Decreased libido and sexual satisfaction
These symptoms can have a significant impact on a woman's overall well-being, self-esteem, and quality of life. It's essential to address GSM promptly to prevent further complications and maintain overall health and vitality.
Managing Genitourinary Syndrome of Menopause
While GSM is primarily caused by hormonal changes during menopause, a multifaceted approach combining medical treatments, lifestyle modifications, and personalized support can help alleviate symptoms and improve overall well-being.
Hormone Therapy
For many women, hormone therapy (HT) is an effective treatment option for managing GSM symptoms. HT can be administered in various forms, including oral medications, vaginal creams, rings, or tablets. It helps restore the vaginal tissue's elasticity and moisture by replenishing the body's estrogen levels.
However, it's crucial to discuss the potential risks and benefits of hormone therapy with a healthcare provider, as it may not be suitable for all women, particularly those with a history of certain medical conditions such as breast cancer or cardiovascular disease.
Non-Hormonal Treatments
For women who cannot or prefer not to use hormone therapy, there are non-hormonal treatment options available. These include:
Vaginal estrogen therapy: Low-dose vaginal estrogen creams, rings, or tablets can help alleviate GSM symptoms without significantly increasing systemic estrogen levels.
Ospemifene: This oral medication, a selective estrogen receptor modulator (SERM), can help improve vaginal dryness and dyspareunia.
Laser therapy: Fractional CO2 laser therapy or vaginal rejuvenation procedures can stimulate the production of collagen and improve vaginal tissue health.
Vaginal moisturizers and lubricants: Over-the-counter vaginal moisturizers and lubricants can provide temporary relief from dryness and discomfort during sexual activity.
Lifestyle Modifications
While medical treatments are essential for managing GSM symptoms, incorporating lifestyle modifications can also play a crucial role in overall well-being during menopause.
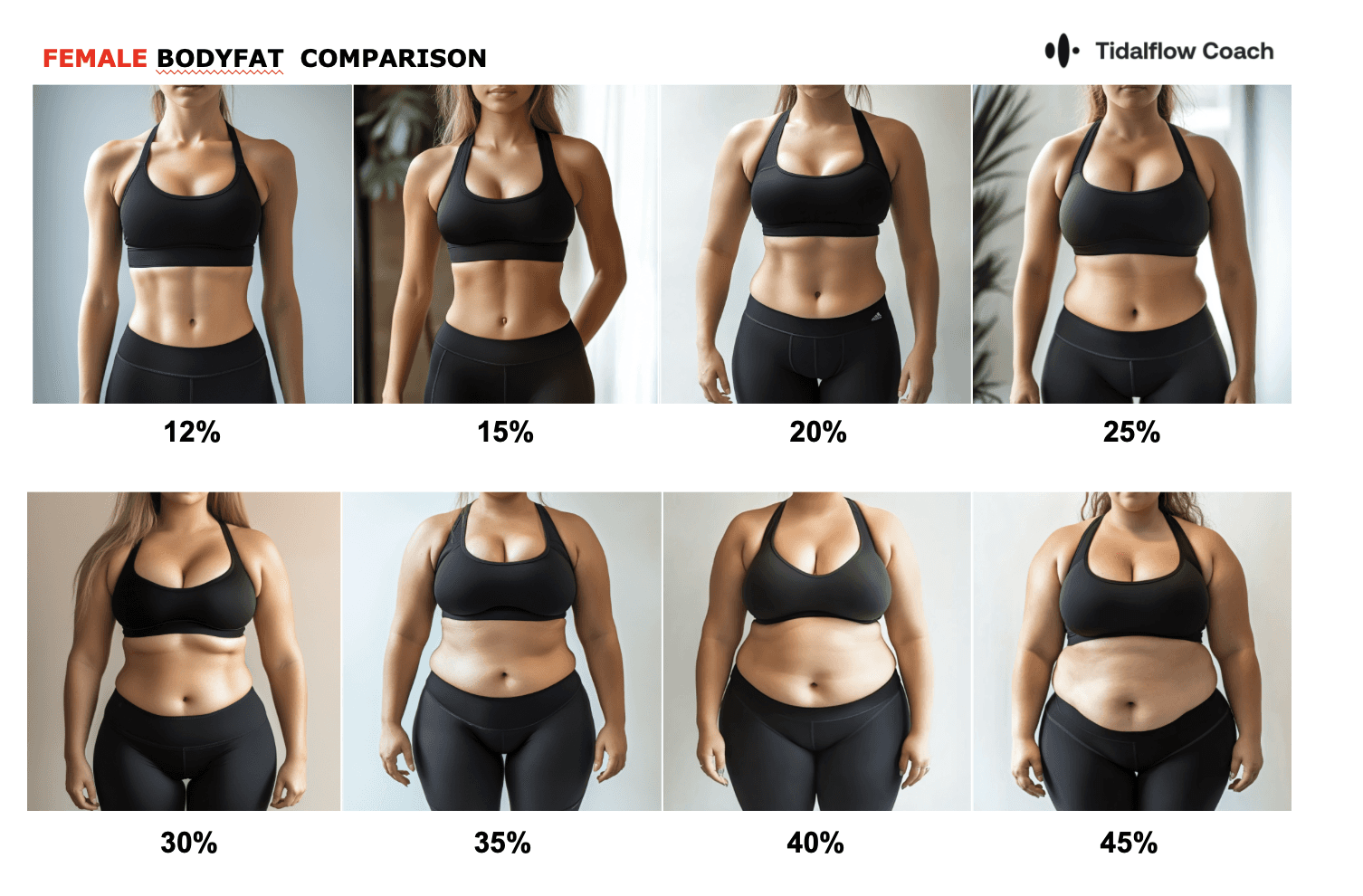
Regular exercise: Maintaining a healthy body weight and engaging in regular physical activity can improve blood flow, promote better sleep, and reduce stress levels, all of which can contribute to managing GSM symptoms more effectively.
Pelvic floor exercises: Strengthening the pelvic floor muscles through Kegel exercises can help improve bladder control and reduce urinary incontinence, a common symptom of GSM.
Stress management: Menopause can be a stressful time, and stress can exacerbate GSM symptoms. Incorporating stress management techniques, such as mindfulness practices, breathing exercises, and relaxation strategies, can help you cope with the physical and emotional changes associated with this phase.
Nutrition: Proper nutrition plays a crucial role in maintaining overall health during menopause. A diet rich in phytoestrogens, found in foods like soy, flaxseeds, and certain fruits and vegetables, may help alleviate some GSM symptoms.
The Role of Personalized Support and Getlila's AI-Powered Solutions
While managing GSM requires a multifaceted approach, having personalized support and guidance can make a significant difference in your journey towards restoring vitality and well-being. At Getlila, our AI-powered personal training solutions are designed to provide tailored support and empower women navigating the challenges of menopause, including GSM.
Tailored Exercise Programs
Our AI personal trainers can create customized exercise programs that cater to your specific needs, fitness levels, and goals. Regular physical activity can help improve cardiovascular health, strengthen muscles, promote better sleep, and reduce stress – all of which can contribute to managing GSM symptoms more effectively.
Nutrition Guidance
Proper nutrition is crucial for maintaining overall health during menopause and managing GSM symptoms. Our AI trainers can provide personalized meal plans and nutritional guidance to help you make informed choices about your diet, including recommendations for foods rich in phytoestrogens and other beneficial nutrients.
Stress Management Techniques
Stress can exacerbate GSM symptoms and negatively impact overall well-being. Our AI trainers can guide you through various stress management techniques, such as mindfulness practices, breathing exercises, and relaxation strategies, to help you cope with the physical and emotional changes associated with menopause.
Personalized Support and Accountability
One of the key advantages of Getlila's AI-powered solutions is the personalized support and accountability they provide. Our AI trainers will work closely with you, monitoring your progress, providing feedback, and adjusting your program as needed to ensure you achieve your goals and maintain a healthy, fulfilling lifestyle.

Conclusion
Genitourinary syndrome of menopause is a common condition that can significantly impact a woman's quality of life, but it doesn't have to be a silent struggle. By understanding the causes, symptoms, and available treatment options, and embracing a holistic approach that combines medical treatments, lifestyle modifications, and personalized support, women can effectively manage GSM and reclaim their vitality and well-being.
At Getlila, we believe in empowering women to navigate the challenges of menopause with confidence and support. Our AI-powered personal training solutions offer a comprehensive approach, combining tailored exercise programs, nutritional guidance, stress management techniques, and personalized support to help you manage GSM symptoms and thrive during this transitional phase.
Embrace this journey with Getlila, and experience the transformative power of personalized fitness solutions. Get started today and take the first step towards restoring your vitality and well-being.
Ready to Simplify Weight Loss?
Download the Lila app or visit getlila.com to start your journey. Experience the power of an AI-driven approach designed to adapt to your changing body and unique needs. Embrace holistic weight loss with Lila—because you deserve to feel strong, confident, and truly yourself again.
Disclaimer: This article is for informational purposes only and does not substitute professional medical advice. Consult a healthcare provider for personalized recommendations.
You should not have to do it all on your own